Everything You Know About Cholesterol Is Wrong
- The traditional view of cholesterol and heart disease is backwards. New research shows that cholesterol seems to be a symptom of heart disease, not a cause.
- Inflammation is what damages arterial walls and contributes to cardiovascular problems. Cholesterol is the repair molecule that comes in and tries to fix the damage. You should be more concerned about inflammation, not high cholesterol.
- Read on for 5 ways to decrease your inflammation, improve your arteries, and boost your performance.
“The more I reviewed the literature, the more I realized, ‘You know what? It seems like everything they teach us in nursing school, in medical school, in pharmacy school about lipids, about LDL, about VLDL, and HDL, the good cholesterol, the bad cholesterol, and how the stuff works — it’s probably wrong, or at least incomplete.”
That’s Zubin Damania, a primary care clinical director and internal medicine doctor at Stanford. Dr. Damania sat down with Dave Feldman, an engineer turned cholesterol expert, to talk about why your cholesterol numbers don’t mean what you’ve been told they do.
Feldman started a ketogenic diet and his cholesterol went up to over 300 mmol/L, with his LDL (“bad cholesterol”) number around 260. For reference, traditional guidelines say your LDL should be under 100, and total cholesterol, below 200.
Feldman was confused, because he’d lost weight, his other health markers were way up, and he felt better than he ever had in his life. So, like any good engineer, he began to investigate. Feldman has spent the last few years of his life learning about the cholesterol system and collecting personal data about how a low-carb diet affects his cholesterol.
He published his experiments and data on his website, where readers began to take notice. Over 50 people have submitted their own data, developing a growing body of evidence that cholesterol is misunderstood, especially when it comes to low-carb, high-fat diets.
In the interview linked below, Feldman and Damania talk about a new theory of cholesterol: that its role in heart disease is misunderstood, and that the real thing you want to worry about is inflammation.
None of this is medical advice, and you should always consult a physician before making changes to your health. That said, here’s an interesting case for why high cholesterol may not be a bad thing, especially if you’re on a low-carb, high-fat diet like the Bulletproof Diet.
How you turn fat into energy on a low-carb diet
 When you’re on a high-carb diet, you get most of your energy from glucose. You eat carbs, digest them into glucose, and send glucose through your bloodstream to hungry cells, with a little direction from insulin. Your blood is mostly water, and glucose dissolves into it with no problem (imagine stirring sugar into a glass of water).
When you’re on a high-carb diet, you get most of your energy from glucose. You eat carbs, digest them into glucose, and send glucose through your bloodstream to hungry cells, with a little direction from insulin. Your blood is mostly water, and glucose dissolves into it with no problem (imagine stirring sugar into a glass of water).
When you’re on a high-fat diet, you get most of your energy from fat. The process starts off similarly to the way carbohydrate metabolism does: you eat fat and digest it into fatty acids.
But you can’t send fatty acids right into your bloodstream because fats and liquids don’t mix. The fat would separate out and wouldn’t go anywhere (imagine stirring oil into a glass of water).
Fats are still a great and efficient source of fuel; your body simply has to be a little more clever in delivering them. Feldman explains it well. “Fatty acids can’t swim in the bloodstream,” he says. “They need containers — sort of like boats — to carry them to cells throughout your body.”
Your body does two things to get fatty acids to energy-hungry cells and power your body:
- It bundles fatty acids into convenient packages of three (called triglycerides), which makes them easier to transport.
- It creates “boats” to drive the triglycerides around your body. These boats are called lipoproteins. Lipoproteins with a full load of triglyceride passengers are very-low-density lipoproteins (VLDL), while lipoproteins that have already dropped off their triglycerides are low-density lipoproteins (LDL).
Does LDL sound familiar? Maybe from your last cholesterol test?
What is LDL cholesterol?
 LDL is what a lot of traditional doctors call “bad cholesterol.” Ironically, LDL isn’t even cholesterol. It’s a big container that carries valuable fat-based compounds throughout your blood. Cholesterol is only one of many passengers in LDL, and if you’re in good shape, it rarely leaves the boat.
LDL is what a lot of traditional doctors call “bad cholesterol.” Ironically, LDL isn’t even cholesterol. It’s a big container that carries valuable fat-based compounds throughout your blood. Cholesterol is only one of many passengers in LDL, and if you’re in good shape, it rarely leaves the boat.
“Calling LDL ‘cholesterol’ would be like naming a boat after its life rafts,” Feldman says. LDL particles really only have cholesterol with them in case of emergencies, because one of cholesterol’s main functions is cellular repair.[1]
LDL mostly exists to carry fat-based energy to your cells. No surprise, then, that LDL goes up when you’re on a high-fat diet. You actually want more LDL — you have more fatty acids to carry through your bloodstream and deliver to your cells for fuel, and you need LDL to do it. And if you’re in good shape and don’t need constant cellular repair, the leftover cholesterol gets packaged into high-density lipoprotein (HDL) particles and sent to your liver to make sex hormones (one reason a high-fat diet is good for increasing testosterone).
“That’s the genius of the human body,” Feldman says. “It has a kind of FedEx for all the [fat-based] elements needed by the cells. And most of what isn’t used gets recycled by the liver for many other possibilities, such as hormone or bile salt production.”
If you’re running on fat for fuel, it makes sense that you’ll have higher numbers on a cholesterol test. If your body isn’t in constant need of repair, you’ll use the extra cholesterol to balance your hormones and improve other essential functions in your body.
Inflammation causes heart disease, not cholesterol
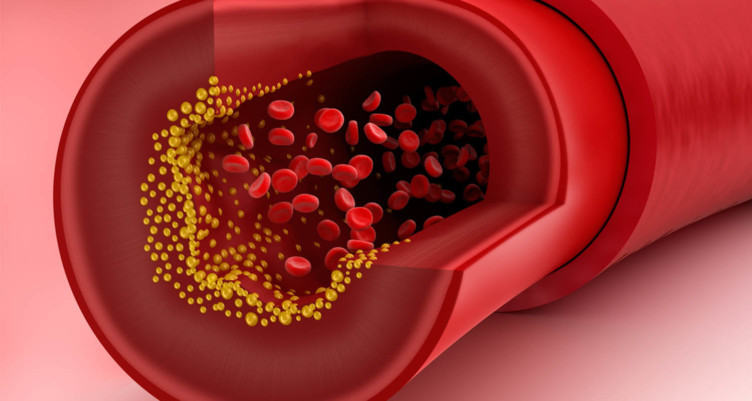
 A common misconception is that cholesterol builds up and “clogs your arteries,” like grease blocking a pipe. The process is more nuanced than that.
A common misconception is that cholesterol builds up and “clogs your arteries,” like grease blocking a pipe. The process is more nuanced than that.
As you read about in the last section, cholesterol is a repair molecule that shows up to heal damaged cells. When your arterial walls get damaged, cholesterol arrives to fix the problem. The issue is that LDL particles carrying cholesterol are large, and they can get stuck in the tear in your arterial wall. That’s when plaques begin to form.
The solution, then, shouldn’t be to decrease your LDL and deprive your body of repair. It should be to get rid of whatever’s tearing holes in the walls of your arteries. LDL is a symptom of an underlying problem, not a cause. The question is, what causes arterial damage in the first place?
The answer seems to be inflammation.
“One of my favorite examples is smoking,” Feldman says. “Smoking causes oxidative stress that damages endothelial [artery] cells…the damaged cells then become problematic, to the extent that it makes sense that the body would take action to repair them. Would you rather have a hole in the endothelial wall of your blood vessel, or would you rather have some spackle there to try to plug the leak?”
Cholesterol seems to be a symptom of a larger problem. So why the confusion all these years about cholesterol causing heart disease?
It’s a perfect example of correlation not being causation. The most influential study in figuring out risk factors for heart disease is the Framingham Heart Study. It started back in the 1940s, following people over several generations and collecting data on their heart health. The Framingham Study has been a wealth of knowledge when it comes to learning about heart disease, but some of the data could be misconstrued.
The Framingham Study and related studies have found that the main risk factors for heart attack are:
- High cholesterol (LDL) and arterial plaques
- Smoking
- Obesity
- Lack of exercise
- High blood pressure
- Psychological stress
What’s interesting is that everything on this list (except LDL cholesterol) causes or correlates with inflammation: smoking,[2] obesity,[3] lack of exercise, high blood pressure,[4][5] and psychological stress.[6] And inflammation causes damage to artery walls.[7]
It seems very possible that cholesterol plaques are the result of a highly inflammatory lifestyle. The chronic inflammation tears up your arteries. Then cholesterol shows up to repair them, gets stuck in the tears, and ends up taking the blame for heart disease.
The inflammatory theory of heart disease is becoming more and more mainstream. Researchers have begun to question their initial assumptions about the Framingham study, considering which of the above risk factors are causes of heart disease and which ones are symptoms.[8]
Feldman is one of the biohackers taking cholesterol research into his own hands. You can read more about Feldman’s work on his website, or watch his interview about cholesterol.
5 ways to decrease inflammation (without worrying about your cholesterol)
While there’s still more work to do, it seems pretty clear that chronic inflammation from poor diet, obesity, smoking, lack of exercise, and mental stress is not good for you — no matter how you feel about cholesterol. Here are five ways to help you decrease inflammation, protect your heart, and perform at your best:
Avoid sugar and excess carbs
 Replace carbs (especially refined carbs) with plenty of healthy, unoxidized fat, high-quality protein, and green veggies. You’ll feel the difference.
Replace carbs (especially refined carbs) with plenty of healthy, unoxidized fat, high-quality protein, and green veggies. You’ll feel the difference.
Eat polyphenol-rich plants
 Polyphenols from colorful plants are rich in antioxidants that protect you from inflammatory damage. Aim for a mix of dark green, blue, purple, and red plants. Your plate should be mostly vegetables at every meal.
Polyphenols from colorful plants are rich in antioxidants that protect you from inflammatory damage. Aim for a mix of dark green, blue, purple, and red plants. Your plate should be mostly vegetables at every meal.
Exercise regularly![exercise and heart disease]()
Exercise decreases inflammation long-term, although it causes short-term muscle damage and inflammation that’s necessary for your muscles to grow. Create a routine that combines walking, yoga, and high-intensity interval training.
Cryotherapy

Cryotherapy and cold exposure trigger cold-shock proteins that decrease inflammation and speed up recovery.
Practice meditation

Meditation decreases psychological stress, which in turn lowers inflammation and oxidative damage.
For more cutting-edge advice and ideas on how to biohack your body, sign up for our newsletter below.
Sign up for early access to sales, product launches, the latest Bulletproof news and more!




